ISS Medical Emergency: An Orbital Ambulance Ride
Over the course of its nearly 30 years in orbit, the International Space Station has played host to more “firsts” than can possibly be counted. When you’re zipping around Earth at five miles per second, even the most mundane of events takes on a novel element. Arguably, that’s the point of a crewed orbital research complex in the first place — to study how humans can live and work in an environment that’s so unimaginably hostile that something as simple as eating lunch requires special equipment and training.
Today marks another unique milestone for the ISS program, albeit a bittersweet one. Just a few hours ago, NASA successfully completed the first medical evacuation from the Station, cutting the Crew-11 mission short by at least a month. By the time this article is released, the patient will be back on terra firma and having their condition assessed in California. This leaves just three crew members on the ISS until NASA’s Crew-12 mission can launch in early February, though it’s possible that mission’s timeline will be moved up.
What We Know (And Don’t)
To respect the privacy of the individual involved, NASA has been very careful not to identify which member of the multi-nation Crew-11 mission is ill. All of the communications from the space agency have used vague language when discussing the specifics of the situation, and unless something gets leaked to the press, there’s an excellent chance that we’ll never really know what happened on the Station. But we can at least piece some of the facts together.

On January 7th, Kimiya Yui of Japan was heard over the Station’s live audio feed requesting a private medical conference (PMC) with flight surgeons before the conversation switched over to a secure channel. At the time this was not considered particularly interesting, as PMCs are not uncommon and in the past have never involved anything serious. Life aboard the Station means documenting everything, so a PMC could be called to report a routine ailment that we wouldn’t give a second thought to here on Earth.
But when NASA later announced that the extravehicular activity (EVA) scheduled for the next day was being postponed due to a “medical concern”, the press started taking notice. Unlike what we see in the movies, conducting an EVA is a bit more complex than just opening a hatch. There are many hours of preparation, tests, and strenuous work before astronauts actually leave the confines of the Station, so the idea that a previously undetected medical issue could come to light during this process makes sense. That said, Kimiya Yui was not scheduled to take part in the EVA, which was part of a long-term project of upgrading the Station’s aging solar arrays. Adding to the mystery, a representative for Japan’s Aerospace Exploration Agency (JAXA) told Kyodo News that Yui “has no health issues.”
This has lead to speculation from armchair mission controllers that Yui could have requested to speak to the flight surgeons on behalf of one of the crew members that was preparing for the EVA — namely station commander Mike Fincke and flight engineer Zena Cardman — who may have been unable or unwilling to do so themselves.
Within 24 hours of postponing the EVA, NASA held a press conference and announced Crew-11 would be coming home ahead of schedule as teams “monitor a medical concern with a crew member”. The timing here is particularly noteworthy; the fact that such a monumental decision was made so quickly would seem to indicate the issue was serious, and yet the crew ultimately didn’t return to Earth for another week.
Work Left Unfinished
While the reusable rockets and spacecraft of SpaceX have made crew changes on the ISS faster and cheaper than they were during the Shuttle era, we’re still not at the point where NASA can simply hail a Dragon like they’re calling for an orbital taxi. Sending up a new vehicle to pickup the ailing astronaut, while not impossible, would have been expensive and disruptive as one of the Dragon capsules in rotation would have had to be pulled from whatever mission it was assigned to.
So unfortunately, bringing one crew member home means everyone who rode up to the Station with them needs to leave as well. Given that each astronaut has a full schedule of experiments and maintenance tasks they are to work on while in orbit, one of them being out of commission represents a considerable hit to the Station’s operations. Losing all four of them at once is a big deal.
Granted, not everything the astronauts were scheduled to do is that critical. Tasks range form literal grade-school science projects performed as public outreach to long-term medical evaluations — some of the unfinished work will be important enough to get reassigned to another astronaut, while some tasks will likely be dropped altogether.
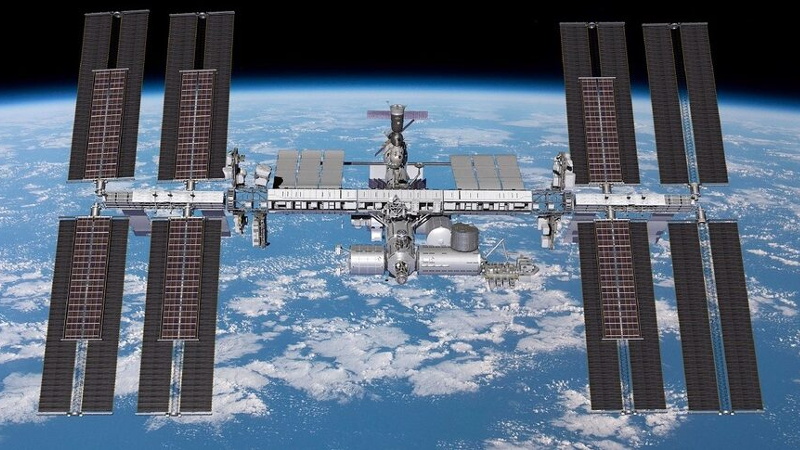
But the EVA that Crew-11 didn’t complete represents a fairly serious issue. The astronauts were set to do preparatory work on the outside of the Station to support the installation of upgraded roll-out solar panels during an EVA scheduled for the incoming Crew-12 to complete later on this year. It’s currently unclear if Crew-12 received the necessary training to complete this work, but even if they have, mission planners will now have to fit an unforeseen extra EVA into what’s already a packed schedule.
What Could Have Been
Having to bring the entirety of Crew-11 back because of what would appear to be a non-life-threatening medical situation with one individual not only represents a considerable logistical and monetary loss to the overall ISS program in the immediate sense, but will trigger a domino effect that delays future work. It was a difficult decision to make, but what if it didn’t have to be that way?

In other timeline, the ISS would have featured a dedicated “lifeboat” known as the Crew Return Vehicle (CRV). A sick or injured crew member could use the CRV to return to Earth, leaving the spacecraft they arrived in available for the remaining crew members. Such a capability was always intended to be part of the ISS design, with initial conceptual work for the CRV dating back to the early 1990s, back when the project was still called Space Station Freedom. Indeed, the idea that the ISS has been in continuous service since 2000 without such a failsafe in place is remarkable.
Unfortunately, despite a number of proposals for a CRV, none ever made it past the prototype stage. In practice, it’s a considerable engineering challenge. A space lifeboat needs to be cheap, since if everything goes according to plan, you’ll never actually use the thing. But at the same time, it must be reliable enough that it could remain attached to the Station for years and still be ready to go at a moment’s notice.
In practice, it was much easier to simply make sure there are never more crew members on the Station than there are seats in returning spacecraft. It does mean that there’s no backup ride to Earth in the event that one of the visiting vehicles suffers some sort of failure, but as we saw during the troubled test flight of Boeing’s CST-100 in 2024, even this issue can be resolved by modifications to the crew rotation schedule.
No Such Thing as Bad Data
Everything that happens aboard the International Space Station represents an opportunity to learn something new, and this is no different. When the dust settles, you can be sure NASA will commission a report to dives into every aspect of this event and tries to determine what the agency could have done better. While the ISS itself may not be around for much longer, the information can be applied to future commercial space stations or other long-duration missions.
Was ending the Crew-11 mission the right call? Will the loses and disruptions triggered by its early termination end up being substantial enough that NASA rethinks the CRV concept for future missions? There are many questions that will need answers before it’s all said and done, and we’re eager to see what lessons NASA takes away from today.
